Cataracts: How Surgery Can Impact a Glaucoma Diagnosis

Eye health is a national concern as 12 million Americans over age 40 experience some vision impairment. Cataracts and glaucoma are among the leading causes of blindness and may sometimes present simultaneously in patients. Here we will explore cataracts and glaucoma and how cataract surgery can influence the glaucoma diagnosis.
What is a Cataract?
A cataract is a cloudy growth in the lens of the eye and occurs more commonly in older individuals. At first, a cataract is not noticeable, but over time it can lead to blurry, hazy, or less colorful vision. Those with cataracts may also have trouble reading or completing daily tasks.
Also, there are several types of cataracts:
- Nuclear cataract in the lens: This cataract is the most common among people over 65.
- Cortical cataract in the lens: Growing from the outside to the center of the lens, people with diabetes often develop this cataract type.
- Subcapsular cataract in the back of the lens: This cataract is common among people with diabetes, far-sightedness, or retinitis pigmentosa.
What is Glaucoma?
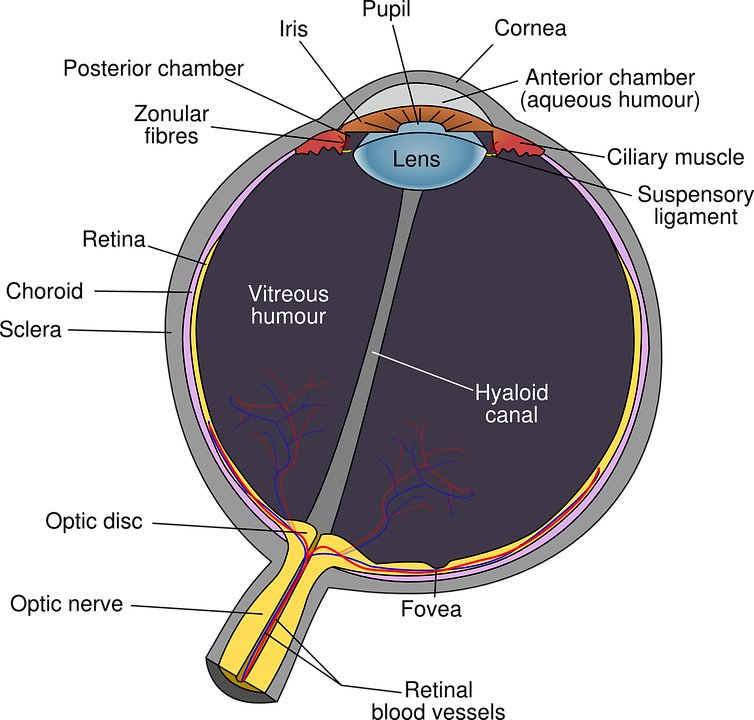
Your eye constantly produces aqueous humor and as new humor flows in, the same volume should drain out via the drainage angle. This process helps to regulate intraocular pressure or IOP. However, if the drainage doesn’t occur, it creates problems.
Glaucoma is a disease that causes fluid to build up in the front part of the eye. That extra pressure damages the optic nerve. The optic nerve consists of over a million tiny nerve fibers (like an electric cable with many wires). As these nerve fibers die, you develop blind spots in your vision. Oftentimes, you don’t notice these issues until it is too late. When all the optic nerve fibers die then blindness occurs.
People of any age can develop glaucoma although it is more common in older adults. Many types of glaucoma have no warning signs and the impact on vision may not be noticeable until the later stages.
When is Cataract Surgery Necessary?
When should you remove cataracts? If you are experiencing significant vision problems and you have a cataract diagnosis, then it may be time to consider surgery.
Surgically removing cataracts is crucial for vision. If left untreated, this condition may result in blindness. However, the right time to surgically address cataracts will vary from one person to the next.
While surgery is available for every stage of cataract progression, it’s important to note the relevant considerations at each stage.
Early Stage Cataracts
A few early signs of cataracts may occur with dysfunctional lens syndrome (DLS) such as glare and halos at night. DLS is often considered a part of the pre-cataract stage. Patients who experience DLS can opt for cataract surgery as soon as the symptoms appear.
A common complaint at this stage is difficulty seeing at night. Therefore, removing a cataract at this stage makes driving at night easier, safer, and more comfortable.
Moderate Cataracts
People with mid-stage cataracts may receive recommendations to help cope with the symptoms before surgery. Some of these recommendations may include stronger corrective lenses or using brighter reading lights. However, cataracts will eventually require surgical removal for complete treatment.
Several doctors recommend having cataracts removed as soon as they become symptomatic. Depending on the progression of cataracts, surgery may be immediately needed or in the future.
Mature Cataracts
Cataracts are more difficult to remove when they become mature. Therefore, many doctors recommend surgery earlier – as soon as vision gets affected regularly.
Furthermore, a mature cataract could lead to significant risks during surgery. This can make the recovery process far longer and more detailed.
However, don’t worry. An experienced cataract surgeon will help you weigh the benefits and risks of cataract surgery – regardless of your current stage.
Financial Considerations of Cataract Surgery
Some insurance companies (such as Medicare) only consider cataract surgery as medically necessary when certain conditions are met. These conditions include reduced visual acuity below 20/40 (the legal vision requirement to drive in most states).
Always review your insurance policy with either an insurance agent or your eye doctor’s staff. Doing so will help you understand if your plan covers the procedure or if you will need to pay out of pocket.
What’s Involved in Cataract Surgery?
You may have wondered how cataract surgery is performed. Good news! We are happy to share the typical surgical procedure to put your mind at ease. Let’s discuss the two main types of surgical interventions:
Phacoemulsification Cataract Surgery
Phacoemulsification is the traditional option for cataract surgery and was introduced 40 years ago. Even now, it is still the most common method to remove cataracts. The surgeon makes incisions (or small openings) in the natural sac (or bag) holding the lens in place. This sac is called the lens capsule. Next, they separate the lens from the lens capsule using a balanced saline solution.
Once the lens is moving freely within the capsule, the surgeon uses a special ultrasound device to break the lens into small pieces and suck it out of the eye. This cataract removal technique is called phacoemulsification.
Before the era of phacoemulsification, the lens was removed in one piece via a large incision of 8 to 12 mm. This fact made for a more risky surgery and a longer recovery window.
After removing the lens, the surgeon injects additional viscous material into the lens capsule to hold it open to facilitate the new artificial lens. The folded artificial lens is inserted into the capsule where it unfolds. The viscous material that maintained the shape of the eye is then removed. These two incisions do not require any stitches and often self-seal with time and care.
Femtosecond Laser (or Laser-Assisted) Cataract Surgery
Femtosecond lasers have been in the ophthalmic surgery rooms since 2001 and during the late 2000s, they were used in cataract surgery. The first laser-assisted cataract surgery was performed in Hungary in 2008.
Once the technique gained FDA approval, the first laser-assisted cataract surgery was performed in the USA in 2010. Since then, the technique has gained acceptance and popularity.
You should note that the laser does not replace manual cataract surgery. The laser simply “helps” to remove the cataract, phacoemulsification breaks down the lens and removes it.
How Does the Laser Work?
The laser serves three critical roles in cataract surgery:
- Makes precise corneal incisions.
- Opens the lens capsule to facilitate removing the cataract
- Initial sectioning of the cataract into smaller pieces
The laser performs these three roles with exceptional precision. Therefore, this aspect makes it better than the surgeon manually performing these tasks. Furthermore, this laser is also used to make corneal incisions to treat certain levels of astigmatism.
Efficiency
Further research is needed to determine if this surgical technique leads to better outcomes and fewer complications compared to phacoemulsification alone. The good news is that much work is underway in this area.
Cost Considerations
Since insurance doesn’t cover the cost of laser-assisted surgery, then you would have to pay a lot out of pocket. Therefore, it is vital to speak with your doctor about the best procedure for your case.
What Are My Lens Implant Options?
An intraocular lens (IOL) replaces the focusing power of your eye’s natural lens. Modern IOLs offer better vision (often without glasses) than before cataract surgery. But, what options are available for your IOL implant?
IOL Options
Your ophthalmologist will perform a complete evaluation of your eyes before recommending an IOL. They will discuss your work, hobbies, and other activities to ensure the IOL fits your lifestyle.
Standard IOLs (Single-Focus)
A standard IOL delivers sharp focusing power at one distance, either near vision (close up) or distance vision (far away). They are also known as single-focus or monofocal lenses.
If you select an IOL designed for near vision, you will need to wear glasses to drive or see objects far away. If your IOL is for distance vision, you wear glasses for reading and other close activities. It’s possible to utilize these lenses in a monovision format. You would have one lens for near vision and the other for distance. However, your eye doctor will help you make the best choice for your needs.
Premium IOLs
Premium IOLs were designated as New Technology Intraocular Lenses (NTIOLs) by the Centers for Medicare and Medicaid Services (CMS). These premium IOLs offer the best possible vision. With these lenses, you won’t need glasses after cataract surgery or you may only wear them occasionally.
Types of Premium IOLs
Premium IOLs are used to correct myopia (nearsightedness), hyperopia (farsightedness), and presbyopia (age-related loss of near-focusing ability).
- Multifocal lenses (or multifocal IOLs) offer several rings of varying powers built into each lens. The section of the lens you look through will determine if you see clearly at a near, intermediate, or far distance.
- Accommodative lenses are hinged and work in coordination with the eye muscles. Its design helps the accommodative lens to move forward for near focus and move backward for distance vision.
- Toric IOLs are designed for astigmatism correction since they have varying powers in different meridians in each lens. They also have alignment markings on the lens’ periphery to help the surgeon adjust the lens’ orientation inside the eye for the best astigmatism correction.
- Trifocal IOLs offer an extensive vision range (near, intermediate, and far). This is the leading presbyopia-correcting IOL in several countries.
Learn More About Intraocular Lens Options
Glaucoma Treatment Options
Unfortunately, glaucoma damage is permanent and irreversible. However, medicine and surgery can help to prevent further damage. Some of these medical interventions include:
Medication
Your doctor may recommend eyedrop medication to lower eye pressure. Some of these medications reduce the aqueous humor that the eye produces, while others help to improve the drainage of the fluid.
Although glaucoma medications can help maintain your vision, they may produce side effects such as:
- Itching or burning sensation
- Red eyes or red skin around the eyes
- Changes in your pulse and heartbeat
- Changes in your energy level
- Changes in breathing (especially for those with asthma or breathing problems)
- Dry mouth
- Blurred vision
- Eyelash growth
- Changes in your eye color, eyelid appearance, or skin around your eyes
All medications can have side effects and can cause problems when taken with other medicines. Therefore, always let your doctor know about all the medications you take regularly to avoid issues.
However, you should never change or stop taking your glaucoma medications without first consulting your eye doctor. If you are about to run out of medication, also speak to your doctor to get a prescription refill.
Laser Surgery
Laser surgery helps to drain aqueous humor from the eye and is often done in an eye doctor’s office or an outpatient center. Two types of laser surgeries can treat glaucoma:
- Trabeculoplasty: The surgeon uses a laser to make the drainage angle work better to ensure the fluid flows out properly to reduce eye pressure.
- Iridotomy: A laser is used to create a tiny hole in the iris to help the fluid flow to the drainage angle.
Operating Room Surgery
Some glaucoma surgery is done in an operating room. This procedure creates a new drainage channel for aqueous humor to leave the eye.
- Trabeculectomy: The surgeon cuts a tiny flap in the sclera and also creates a pocket-like bubble in the conjunctiva called a filtration bleb. This bleb is usually hidden under the upper eyelid. Aqueous humor then drains out of the eye via the flap and into the bleb. Once in the bleb, the fluid gets absorbed into the tissue around the eye, lowering the eye pressure.
- Glaucoma drainage devices: Your ophthalmologist may implant a tiny drainage tube in your eye. This tube sends the fluid into a collection area called a reservoir. This reservoir is created beneath the conjunctiva where the fluid gets absorbed into nearby blood vessels.
Cataract Surgery and Glaucoma
Cataract surgery can improve glaucoma. These patients have narrow angles since the iris and cornea are often too close and they block the eye’s drainage channel. Cataract surgery involves removing the natural lens. This process creates more space for the excess aqueous humor to leave the eye and lower the intraocular pressure (IOP).
This lowered IOP reduces the patient’s reliance on glaucoma medication. Furthermore, the lower IOP could halt optic nerve damage and vision loss. But since every patient’s case is unique, your cataract surgeon will make the best recommendations for your case.
Your surgeon may recommend a joint cataract and glaucoma surgery to help treat your glaucoma. Alternatively, they may recommend only doing cataract surgery to see the positive impact on your glaucoma. The treatment management in such a case is completely different from that of patients who only remove cataracts and have no glaucoma.
Frequently Asked Questions (FAQs)
Can a person have glaucoma and cataracts simultaneously?
It is possible to have glaucoma and cataracts at the same time. In many cases, the two conditions may be unrelated but may be discovered simultaneously. Therefore, your surgeon may recommend and carefully coordinate treatment plans to ensure your best health and minimize the possibility of further vision loss.
Which condition is more severe: glaucoma or cataracts?
Glaucoma can lead to irreversible blindness, whereas vision loss is less likely with cataracts (although it’s possible). Vision loss arising from cataracts is reversible with surgery, but that’s not possible with glaucoma surgery. Therefore, glaucoma is more severe.
Can I undergo cataract surgery with glaucoma?
While every individual’s condition is different, it is often safe to have cataract surgery with glaucoma. Some surgeons may recommend having both procedures done simultaneously.
Get Expert Eye Healthcare
Do you or a loved one need help with cataracts or glaucoma? Ophthalmic Consultants has expert cataract surgeons bringing particular expertise with complex cataract surgery in glaucoma patients. You can depend on us to guide you through a customized treatment plan for optimal results. Contact us today to schedule an initial appointment and begin the journey to better eye health.