Eye Healthcare: How Severe are Retinal Tears and Detachment?

By Dr. David Rabady
Our eyes are among our vital organs and help us to enjoy the world around us. The retina is a crucial part of the eye that facilitates vision. However, retinal tears and detachment have adverse impacts. We will discuss the implications of these eye conditions in this article.
What is a Retinal Tear?
The retina is the thin layer of tissue lining the back of the eye along its interior. Its location near the optic nerve makes it ideal for receiving light and sending pictures to the brain of what the eye sees.
The retina processes light input via its photoreceptor or light-sensitive cells. These cells detect light stimuli, which are interpreted as images, and passed on as visual info to the brain via the optic nerve. The brain then sorts the info and “develops” the pictures.
A retinal tear may lead to fluid and blood collection in the eye. This can result in the development of new floaters that interfere with clear vision. Should the tear devolve into a retinal detachment, it could lead to complete vision loss.
The retina is essential for vision and any extensive damage to it can lead to vision loss and permanent blindness. If the retina can’t receive and process light, then the brain won’t receive any information. A retinal detachment is like a camera with no film — you can’t develop any images.
Retinal Tear Symptoms
The most common symptoms of retinal tears include light flashes and visible spots called floaters. Retinal tears can develop and progress fast and may result in retinal detachment. Other possible symptoms include:
- A sudden increase in the size and number of floaters (a possible indicator that a retinal tear is occurring)
- A sudden appearance of light flashes (the first stage of a retinal tear or detachment)
- Having a shadow appear in your peripheral (side) field of vision
- Seeing a gray curtain slowly moving across your field of vision
- Experiencing a sudden decrease in vision, including focusing trouble and blurred vision
- Having a headache
However, in quite a few instances, a retinal tear may not have any noticeable symptoms.
Retinal Detachment
A retinal detachment is a medical emergency! If you notice any retinal tear symptoms and you begin to lose your vision, contact your eye doctor immediately. Any delay in treatment could worsen your outcome.
Retinal detachment involves the complete lack of attachment of the retinal tissue along the back of the eye. This condition is more severe than retinal tears. Please note that the longer a detached retina remains detached, the higher the risk of permanent vision loss.
Causes of Retinal Detachment
A retinal detachment is a more severe consequence of retinal tears. The vitreous gel (or vitreous humor) is a clear, jelly-like substance that fills most of the interior of the eye. These conditions arise when the vitreous gel inside the eye contracts, tearing away the retina from the eye wall. This contraction of the vitreous gel can occur slowly over time or suddenly.
The primary function of this vitreous gel is to help the eyeball keep its spherical shape during fetal development. However, after the eye develops in utero, the purpose of vitreous gel is unknown.
Types of Retinal Detachment
There are three main types of retinal detachment:
Exudative
This type of detachment arises from conditions, such as inflammatory disorders, and other retinal diseases. In this case, the fluid leaks under the retina even without breaks or tears in the retina.
Rhegmatogenous
This form of retinal detachment occurs when a retinal tear allows fluid underneath it. As the fluid builds up under the retina, it separates from the cell layer (located in the eye’s back wall) and loses its nourishment.
Tractional
In this case, scar tissue on the retina’s surface contracts. Through this contraction, the retina detaches from the back wall of the eye. This is most common with Diabetes, trauma, and other eye surgeries.
The Risk Factors for Retinal Tears and Detachment
Some of the risks of these conditions are:
- Extreme myopia (nearsightedness)
- Previous retinal detachment or tears
- Previous eye injury
- Previous severe eye disease
- Previous eye surgery
- A family history of retinal detachment
- Advanced age (commonplace in people age 50 and older)
Associated Conditions
Some of the conditions associated with retinal tears and retinal detachment include:
- Diabetes
- High myopia (nearsightedness)
- Sickle cell disease
- Scar tissue
- Past eye trauma
- History of retinal tear or detachment
- Retinal degeneration
- Inflammatory disorders
- Autoimmune diseases
- Certain cancers
- Certain hereditary eye conditions
- Retinopathy of prematurity (ROP)
Usually after age 50, the vitreous gel naturally starts to separate from the back of the eye. This is also known as posterior vitreous detachment (PVD) and it increases the risk of retinal detachment.
How to Diagnose Retinal Detachment
Your eye doctor will perform a comprehensive eye exam to diagnose any retinal conditions. In most cases, there are no visible signs of retinal detachment from the outside.
The good news is that this thorough examination allows your doctor to see signs of a tear using ophthalmoscopy. Your doctor will use eye drops to dilate your pupils. Next, they use a special ophthalmoscope to get a three-dimensional view to examine the eye’s interior.
The doctor may also use a slit lamp that magnifies the eye many times. It also illuminates the eye with a bright light so individual structures can be examined. Traces of pigment or blood cells may be detected floating within the vitreous and aqueous field.
Retinal tears and detachment are often visualized during the examination. In some cases, blood may obstruct the view and make it challenging to examine the retina. In such cases, an ultrasound device may be used to examine your eye (especially if there is a lot of bleeding inside the eye). This ultrasound device produces sound waves that bounce off the back of the eye, creating a picture that aids your doctor in determining whether or not your retina is torn or detached.
Retinal Tears and Detachment Treatment Options
A surgical procedure can repair a retinal tear. Your eye doctor will discuss the best type of procedure depending on the extent of the tear. They will also inform you of the various risks and benefits of the possible treatment options.
Treatment Options
Promptly treating a retinal tear generally results in a very good prognosis. Many retinal tears are treated by resealing the retina onto the eye’s back wall using either laser photocoagulation or retinal cryopexy.
Both procedures create a scar that aids in sealing the retina to the back of the eye. This seal prevents fluid from moving through the tear and under the retina. The procedure often prevents the retina from completely detaching.
Your eye doctor will generally perform the treatment in their office, which tends to cause little to no discomfort.
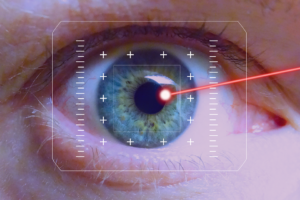
Laser Photocoagulation
Your doctor will use a laser to make small burns around the retinal tear. The resulting scarring will seal the retina to the underlying tissue and prevent retinal detachment.
Cryopexy
Your doctor will use a freezing probe to freeze the retina around the retinal tear. The result is a scar that secures the retina to the eye’s back wall. This is an older technique and not used as widely.
The following treatment options are most suitable for cases of retinal detachment:
Vitrectomy
For this surgery, the doctor will create three tiny incisions in the white part of your eye. Then, using small instruments, they guide and extract the vitreous fluid collected underneath your retina.
The surgeon will then place a bubble of gas or silicone oil in the eye. This insertion pushes the retina to the eye’s back wall. Then, they will use laser photocoagulation to seal the retinal break.
Over a few weeks, you will naturally absorb the gas into your body. This leaves space for the natural eye fluids to refill your eye. However, if silicone oil is used, the surgeon will have to perform another procedure in a few weeks to extract.
Pneumatic Retinopexy
Pneumatic retinopexy is most suitable for cases of small detachment due to a single tear at the top of the retina. In this procedure, the eye surgeon will inject a tiny gas bubble inside your eye to plug the retinal tear and fix the detachment.
Plugging the tear helps the fluid to collect at the back of the retina, get reabsorbed into the eye, and help the retina reattach. It could take a few days before the retina adheres properly. Once that happens, the surgeon closes the retinal tear using laser photocoagulation or cryopexy. The gas bubble then self-reabsorbs over a few weeks.
Scleral Buckling
With this surgery, your eye surgeon attaches a silicone band (buckle) to the sclera (the white part of your eye). But, before doing so, they will drain the fluid from underneath your retina and then suture in the buckle.
What’s the role of this buckle? It counteracts the force pulling your retina forward, applying gentle pressure to push the retina back into the eye’s back wall for healing and reattachment in its normal position.
After securing your retina back into its correct position, the surgeon uses laser photocoagulation to “weld” shut the edges of the retinal tear and seal the leak.
Recovery After Retinal Detachment Surgery
You must get lots of rest post-surgery. Your eye doctor will prescribe eye drops to help with recovery and prevent complications. They may also give you an eye shield or a patch to wear over your eye, which you will need to wear for a few days.
What to Expect During Recovery
As you recover, you will experience blurred vision, some eye discomfort, and red, swollen, or tender eyes.
If the surgeon used a gas bubble to flatten the retina back into the eye’s wall, there are further instructions. They will advise you to ensure your head is in a particular position for a certain number of days. After that, it will take another two to four weeks before you can resume your daily routine.
Follow-up care is crucial for your complete recovery and well-being. Ensure that you attend all scheduled follow-up appointments.
However, if you notice any of these signs, contact your doctor immediately:
- Thick discharge from your eye
- A fever
- Sudden shortness of breath or chest pain
- Abrupt vision changes
- Severe eye pain
- Experiencing new flashes of light in either eye
Retinal detachment is a severe vision-threatening condition requiring prompt treatment by a retinal specialist. Our experienced, board-certified ophthalmologists at Ophthalmic Consultants will be happy to assist you in safeguarding your vision.
How to Stop a Retinal Tear From Worsening into a Detachment
Although retinal tears are dangerous on their own, these tears can degrade into retinal detachment (which is an emergency that can result in blindness). But getting prompt treatment can stop a retinal tear from worsening.
You need to know your risk factors and warning signs so that you can take quick action to preserve your vision. Our team of experienced ophthalmologists at Ophthalmic Consultants can provide world-class eye examinations, treatments, and guidance to help keep your eyes healthy.
Here are a few things to consider to prevent a retinal tear from devolving into a retinal detachment:
Know the Warning Signs
Almost all of us experience the occasional floaters – those gray and transparent specks that float across our vision fields. Along with the symptoms of a retinal tear that we have reviewed, it’s essential to know when you experience new symptoms or these symptoms more frequently. That means it’s time to take preventative steps.
Visit an Ophthalmologist
Ophthalmic Consultants offer comprehensive eye exams that include high-tech diagnostic tests. These tests include retinal scans and other tests to detect retinal tears and detachment.
If you have one of these conditions, then the exam will indicate the need for corrective medical interventions. We perform photocoagulation, cryopexy, or surgeries like vitrectomy to repair the retina and safeguard your vision.
Prompt action is crucial as the faster you access treatment, the better your outlook. Do all you can to preserve your vision and prevent any worsening of your eye health.
Take Care of Your Eyes: You Only Have One Pair!
When you protect your eyes, you minimize the risk of retinal failure and other eye conditions. For example, always wear protective goggles when completing DIY projects and playing high-contact sports such as baseball, hockey, or lacrosse.
Furthermore, you need to take care of your overall health and ensure you control any conditions such as high blood pressure and diabetes. Also, eating a healthy diet and getting at least 30 minutes of moderate exercise daily will greatly improve your health.
Schedule routine eye exams even if you don’t need glasses or contacts. Most eye diseases (such as retinal weakness or vitreous changes) have no symptoms in the early stages. However, getting our eye experts on board will ensure that we diagnose and treat all your health conditions before they get worse.
Get Expert Assistance to Safeguard Your Vision
We have reviewed retinal tears and detachment at length and offered critical signs that may indicate their presence. Have you or your loved ones experienced any symptoms? Contact Ophthalmic Consultants to get expert opinions on your eye health and ample guidance if any interventions are necessary. We invite you to schedule an appointment and preserve your vision and lifestyle.